The patient was apparently asymptomatic 6 months ago when he developed jaundice and was treated at a private practitioner.
Later he developed abdominal distension about 7 days ago - insidious in onset, gradually progressive to the present size - associated with
- Pain in epigastric and right hypochondrium
- Not associated with fever , No night sweats.
- Not associated with Nausea, vomiting, loose stools
There was pedal edema ( grade 2 )
- Gradually progressive
- Pitting type
- Bilateral
- Below knees
- Increases during the day - maximum at evening.
- No local rise of temperature and tenderness
- Not relived on rest
He also complained of shortness of breath since 4 days - MRC grade 4
- Insidious in onset
- Gradually progressive
- Aggravated on eating and lying down ; No relieving factors
- No PND
- No cough/sputum/hemoptysis
- No chest pain
- No wheezing
Patient is a known alcoholic since 20 years, he stopped taking alcohol since 6 months When he drank on 29/5/22 ascites has increased.
Daily Routine :
Wakes up at 5am and goes to field.
Comes home at 8am and has rice for breakfast. Returns to work at 9am.
1pm - lunch
2-6 pm - work
6pm - home
8pm - dinner
Alcohol- 2 times a week, 180 ml.
PAST HISTORY:
No history of similar complaints in the past
Medical history- not a known case of DM, HTN, TB, Epilepsy, Asthma, CAD
Surgical history - not significant
PERSONAL HISTORY:
- Diet - mixed
- Appetite- reduced since 7 days
- Sleep - disturbed
- Bowel - regular
- Bladder - oliguria since 2 days, no burning micturition, feeling of incomplete voiding.
- Allergies- none
- Addictions - Beedi -4 - 5/day since 30 years ;
- Alcohol - Toddy - 1 bottle, 2 times a week, since 30 years;
- Whiskey-180 ml, 2 times a week, since 5 years.
- Last alcohol intake - 29th May, 2022.
FAMILY HISTORY:
Not significant
GENERAL EXAMINATION:
Patient is conscious, coherent and co-operative.
Examined in a well lit room.
Moderately built and nourished
Icterus - present (sclera)
Pedal edema - present - bilateral pitting type, grade 2 No pallor, cyanosis, clubbing, lymphoedenopathy.
Vitals :
Temperature- afebrile
Respiratory rate - 16cpm
Pulse rate - 101 bpm
BP - 120/80 mm Hg.
SYSTEMIC EXAMINATION:
CVS : S1 S2 heard, no murmurs
Respiratory system : normal vesicular breath sounds heard.
Abdominal examination:
INSPECTION :
Shape of abdomen- distended
- Umblicus - everted
- Movements of abdominal wall - moves with respiration
- Skin is smooth and shiny;
- No scars, sinuses, distended veins, striae.
PALPATION :
Local rise of temperature present.
Tenderness present - epigastrium.
Tense abdomen
Guarding present
Rigidity absent
Fluid thrill positive
Liver not palpable
Spleen not palpable
Kidneys not palpable
Lymph nodes not palpable
PERCUSSION:
Liver span : not detectable
Fluid thrill: felt
Tympanic note is heard on the midline and dull note is heard on the flanks in supine position
AUSCULTATION:
Bowel sounds are decreased
CNS EXAMINATION:
Conscious
Speech normal
No signs of meningeal irritation
Cranial nerves: normal
Sensory system: normal
Motor system: normal
Reflexes: Right. Left.
Biceps. ++. ++
Triceps. ++. ++
Supinator ++. ++
Knee. ++. ++
Ankle ++. ++
Gait: normal
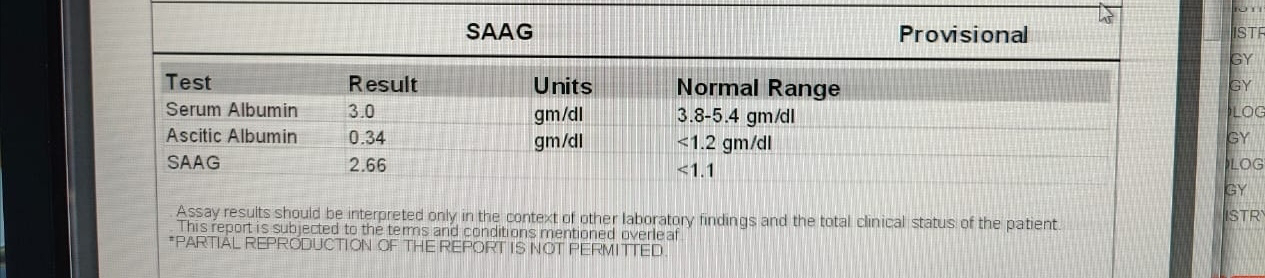
INVESTIGATIONS:
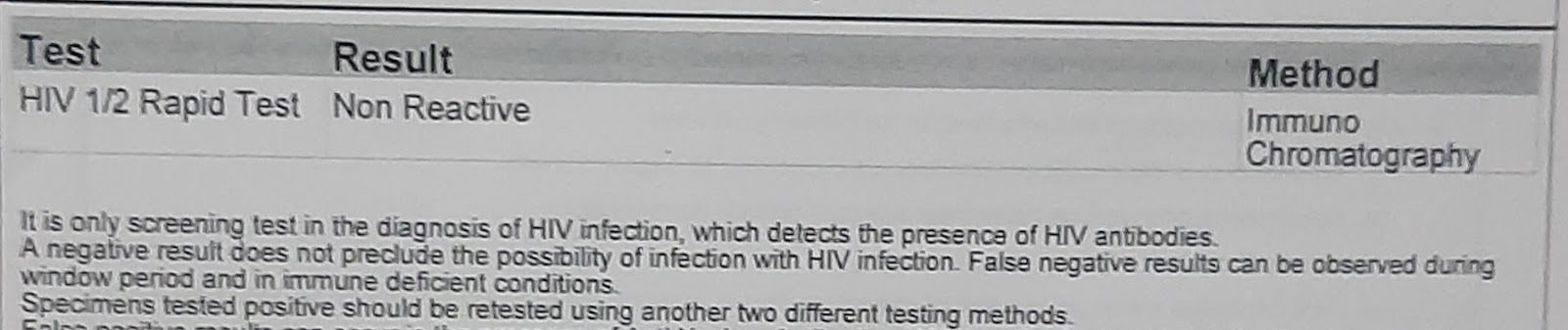
Serology:
HIV - negative
HCV - negative
HBsAg - negative
PROVISIONAL DIAGNOSIS:
Decompensated chronic liver disease with ascites.
TREATMENT:
Inj Lasix 40 mg iv BD
Tab spironolactone 50 mg BD
Paracentesis
Syp. Lactose 15ml TID
Abdominal girth charting - 4th hourly
Fluid restrictriction less than 1L per day
Salt restriction less than 2 gms per day























Comments
Post a Comment